Public, Patients & Caregivers
Sleep is important for several aspects of physical, emotional, and intellectual functions. A considerable proportion of the population has insufficient sleep, an avoidable phenomenon known to worsen mental and physical health, lower productivity, and increase rates of accidents, injuries, and deaths. Sleep needs vary substantially from one person to the next. Even if on average, most people sleep between 7-9 hours, others are naturally “short” or “long” sleepers. It is important to listen to our body and adjust our sleep to get what we personally need to feel well during the day.
-
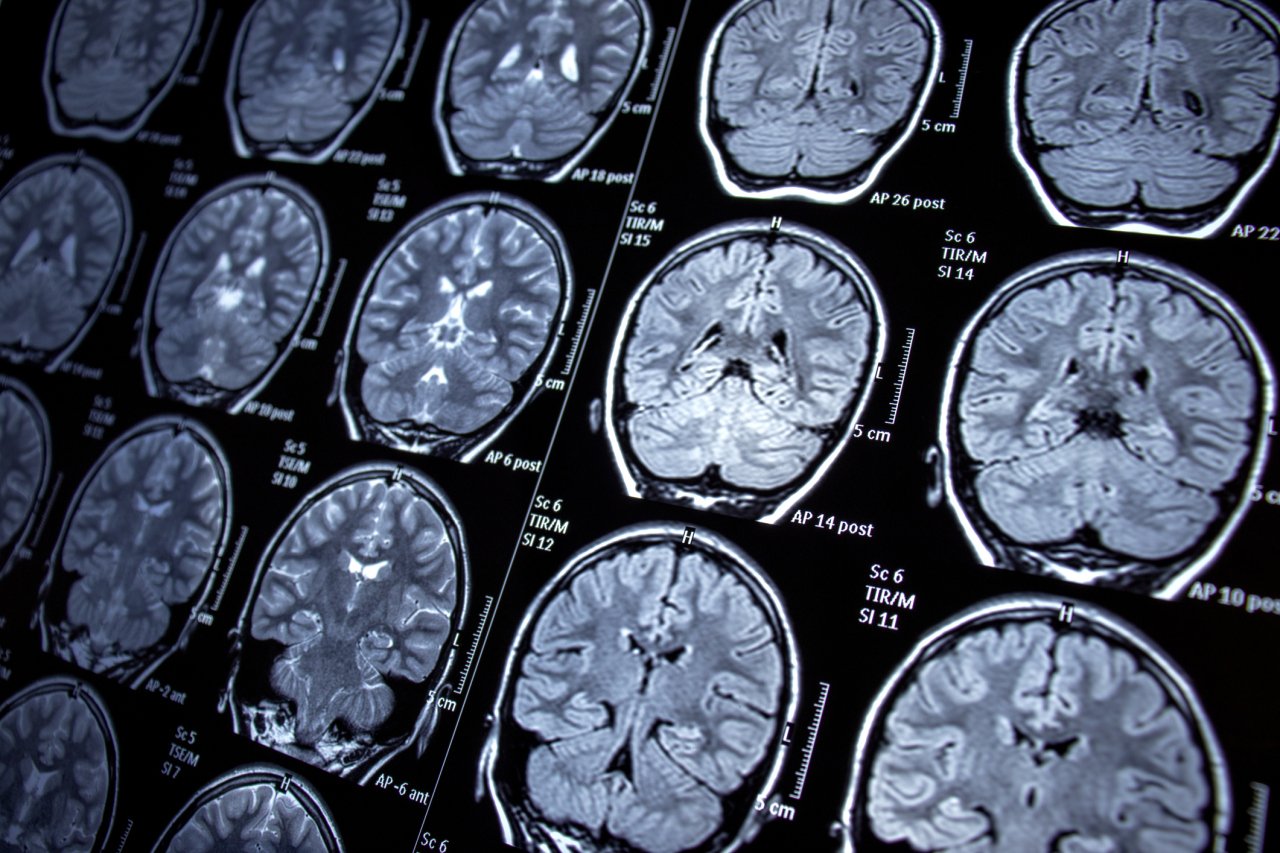
Sleep is in part regulated by the biological clock in our brain. Light is the strongest external signal adjusting the timing of this biological clock. The timing of light exposure is critical: Bright light in the morning helps us wake-up more easily and feel more energized, but light in the evening (like that emitted by electronic devices) suppresses our sleep hormones, making it harder to fall asleep.
Daylight savings time imposes significant challenges to our sleep and biological clock. This practice is notably linked to surges in accidents, heart attacks, pregnancy loss, and mental health problems. Hence, the scientific community unanimously advises to abolish this practice and to stay on standard time permanently (Position statement of the Canadian Sleep Society; recent press article click here).
Sleep changes considerably across the lifespan. It is important to keep realistic expectations about sleep quality and quantity as we age. Yet, since the rates of certain sleep disorders (e.g. insomnia, sleep apnea, restless leg syndrome) do increase with aging, it is important to get assessed and treated if sleep problems interfere with our daily lives.
Menopause imposes another layer of challenges on sleep, notably via increased risks of insomnia, sleep apnea, and sleep difficulties related to anxiety or depression. Tips to better handle sleep challenges linked to menopause include: adjusting our clothes, beddings and room temperature to stay cool, keeping active, and implementing lifestyle changes to protect our sleep (see the 10 rules of sleep hygiene below). Certain medications can also help; talk to your doctor!
There is a bi-directional relationship between sleep and mental health. Addressing sleep problems significantly improves mental health. For example, several studies reported that sleep therapies can attenuate mental health symptoms linked to anxiety, depression, bipolar disorder, and post-traumatic stress disorder.
During the night, there is an imbalance between the emotional parts of our brain (overly active) and the rational parts of our brain (less active), which makes us prone to unhelpful intrusive thoughts that tend to go in circles. For most people, nighttime is not the ideal time to problem-solve; one tip is to note down our concerns to get them out of our minds and deal with them on the next day.
During the COVID-19 pandemic, changes in the duration and timing of sleep paralleled the surge in stress, anxiety and depression symptoms (Infographic - Canadian data on sleep and mental health during the pandemic).
-
View the sleep tips for all ages on our webpage
-
If, after applying the tips above, difficulties to fall asleep or stay asleep persist for a sustained period of time and impact our ability to function during the day, this may be a sign of insomnia disorder. Cognitive-Behavioral Therapy for insomnia (CBTi) is the recommended first line of treatment for insomnia (before or while starting medications). This is typically delivered by psychologists or physicians specialized in sleep.
It is also important to recognize signs of other sleep disorders to see when you should consult a sleep specialist.
For example:
Feeling excessively sleepy during the day, even if we may be sleeping enough during the night
Being told that we stop breathing during the night and/or waking up grasping for air
Discomfort in legs during the evening
Experience frequent nightmares that break down our sleep